An estimated 10 million Americans have osteoporosis, and an additional 34 million are estimated to have low bone mass, placing them at increased risk for developing vertebral compression fractures.
Vertebral compression fractures (VCFs) are the most common fracture in patients with osteoporosis, affecting about 750,000 people annually.
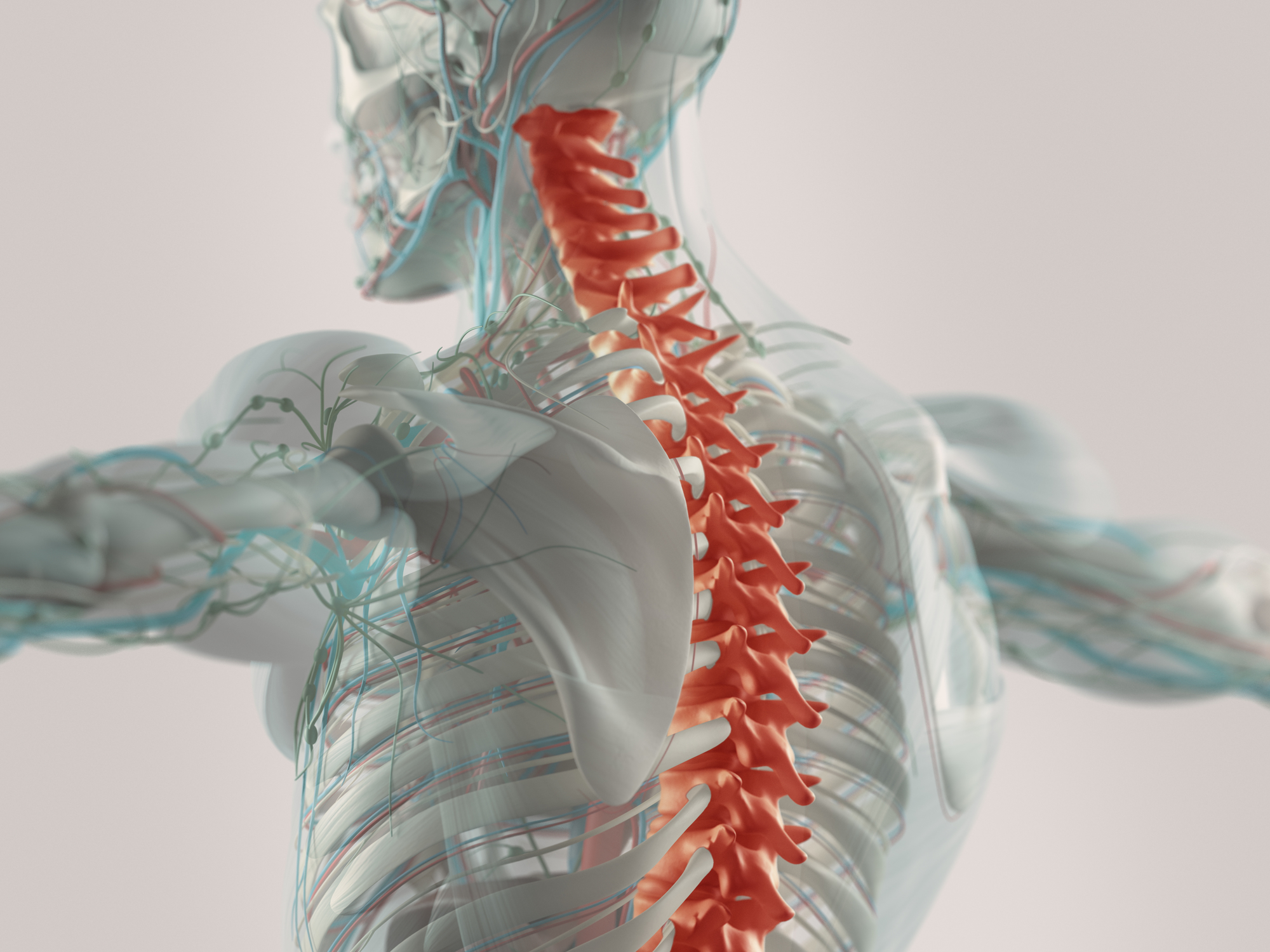
VCFs occur when the bony block or vertebral body in the spine collapses, which can lead to severe pain, deformity and loss of height. While osteoporosis is the most common cause, these fractures may also be caused by trauma or metastatic tumors.
The main clinical symptoms of VCFs may include any of the following, alone or in combination:
- Sudden onset of back pain
- An increase in pain intensity while standing or walking
- A decrease in pain intensity while lying on the back
- Limited spinal mobility
- Eventual height loss
- Eventual deformity and disability
While a diagnosis can usually be made through history and a physical examination, plain x-rays, computed tomography (CT), or magnetic resonance imaging (MRI) can help in confirming a diagnosis, predicting prognosis, and determining the best treatment options.
Traditionally, people with severe pain from VCFs have been treated with bed rest, over-the-counter medications, bracing, use of heat or ice, and a slow return to mobility. Surgery may also be advisable depending upon the servility of the pain and injury. After sustaining a vertebrae fracture, a patient is at risk for more fractures, so treatment of the underlying osteoporosis is an important part of the treatment plan.

